Table of Contents
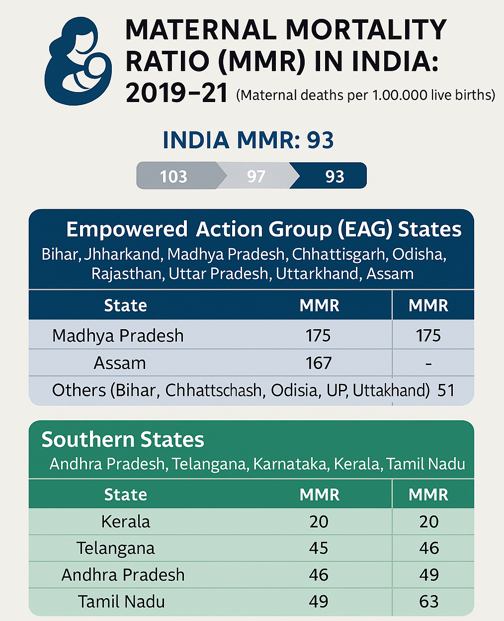
Context: The Maternal Mortality Ratio (MMR) for India is on the decline, but there are States that need to focus on basic and systemic issues.
Maternal Care in India: Challenges
- Three Delays Model: Delay in recognising complications and seeking care (due to low awareness, financial issues, social taboos).
- Delay in reaching a health facility (poor roads, remote areas, lack of ambulances).
- Delay in receiving adequate care at the facility (staff shortages, lack of blood banks, delayed referrals).
- Shortage of Trained Health Professionals: High vacancy rates for specialists (obstetricians, anaesthetists, paediatricians), especially in Community Health Centres and First Referral Units (FRUs).
- Eg., 66% vacancies of specialists in 5,491 community health centres.
- Anaemia and Malnutrition: A large proportion of pregnant women are anaemic or malnourished, increasing the risk of complications and maternal deaths.
- Eg., According to NFHS-5 (2019-21), over 50% of pregnant women in India are anaemic.
- Home Deliveries and Unsafe Abortions: Despite progress, a section of deliveries still happen at home by untrained birth attendants, leading to sepsis, trauma, and increased mortality.
- Socio-cultural and Economic Barriers: Early marriages, low education levels, poverty, and gender inequality hinder timely and safe maternal care.
- Ineffective Maternal Death Audits: Weak implementation of mandatory reporting and audit of maternal deaths in several states limits systemic improvement.
|
Major Government Initiatives Related to Maternal Care |
|||
| Initiative | Launched | Main Focus | Key Features |
| Janani Suraksha Yojana (JSY) | 2005 | Promote institutional delivery | Cash incentives for mothers & ASHAs to deliver at health facilities |
| Janani Shishu Suraksha Karyakram (JSSK) | 2011 | Free maternity and newborn care | Free delivery (incl. C-section), drugs, diagnostics, diet, blood, and transport for mother & newborn |
| PMSMA (Pradhan Mantri Surakshit Matritva Abhiyan) | 2016 | Quality antenatal care | Free specialist ANC on the 9th of every month; focus on early risk detection |
| LaQshya | 2017 | Labour room quality improvement | Upgradation of labour rooms, maternity OTs, staff training, and quality assurance |
| SUMAN (Surakshit Matritva Aashwasan) | 2019 | Dignified, assured maternal-newborn services | Zero expense, respectful, quality care; grievance redressal; covers all public health facilities |
| Anaemia Mukt Bharat (AMB) | 2018 | Reduce anaemia in women and children | 6×6×6 strategy: IFA, deworming, fortified foods, testing, behaviour change, address non-nutritional causes |
Way Forward
- Strengthen the Three Delays Model Response: Increase community awareness of maternal danger signs and the importance of institutional deliveries.
- Expand financial and transport incentives for timely referral and access.
- Ensure rapid response and triage at facilities, with a clear protocol for emergencies.
- Increase Investment in Health Infrastructure: Fill vacancies of obstetricians, anaesthetists, and staff nurses at all FRUs/CHCs.
- Upgrade operation theatres, blood banks, and critical care units at district and sub-district levels.
- Improve Quality of Maternal Death Audits: Mandatory, confidential reviews of every maternal death (e.g., Kerala Model), with accountability and follow-up actions.
| Kerala Model |
| Compulsory to report and review every maternal death, regardless of cause or location (hospital or home). All cases are reported within 24 hours. |
- Focus on Nutrition and Anaemia Control: Strengthen Iron Folic Acid (IFA) supplementation, nutrition counselling, and community-based interventions for adolescent girls and pregnant women.
- Empower Frontline Workers and Women’s Groups: Continue training and incentivising ASHAs, ANMs, and SHGs for community mobilisation and support.


 Particularly Vulnerable Tribal Groups (P...
Particularly Vulnerable Tribal Groups (P...
 Geo-tagging of Buildings During Upcoming...
Geo-tagging of Buildings During Upcoming...
 Gender Gap in Educational Expenditure in...
Gender Gap in Educational Expenditure in...